In this article, I will walk you through what measurement-based care (MBC) looks like in real-life therapy, using a case example from the Centre for Mental and Psychological Health—a leading clinic that uses evidence-based CBT to meet clients where they are.

At its core, successful therapy involves two things:
1. Truly understanding what the client is struggling with.
2. Building a strong connection by finding out what matters most to the client—what motivates them, fuels their energy, and gives them purpose.
When therapist and client work together to identify meaningful goals, it strengthens their relationship and increases the client’s motivation to work toward those goals.
By using reliable tools like questionnaires and symptom trackers, the therapist can:
· Set a starting point (baseline) for treatment.
· Track progress (or setbacks) over time.
· Give the client a clear picture of how far they have come by the end of therapy.
In this article, I will show how MBC worked in the case of “Malcom” (name changed), a man in his 50s dealing with depression, anxiety, attention issues, impulsivity, and some substance use problems. We will look at MBC across four stages:
1. Introducing MBC and setting the baseline.
2. Tracking symptoms and life changes.
3. Handling sudden setbacks.
4. Wrapping up treatment with a visual summary of progress.
Even though it’s important to track symptoms regularly, it doesn’t mean the therapist and client need to spend a lot of time discussing every detail of the results.
Setting the Baseline
At the start of therapy, once the assessment is done, the therapist explains MBC to the client—why it is used, how it helps, and what is expected between sessions. The first set of questionnaires creates a baseline to compare future progress.
The therapist takes time to answer any questions to make sure the client understands and is willing to participate. This step is crucial because the client’s commitment depends on believing that these tools are useful.
For Malcom, the conversation went something like this:
“Here at the clinic, we monitor your symptoms and how well you are functioning. Each week, I will ask you to fill out three short questionnaires:
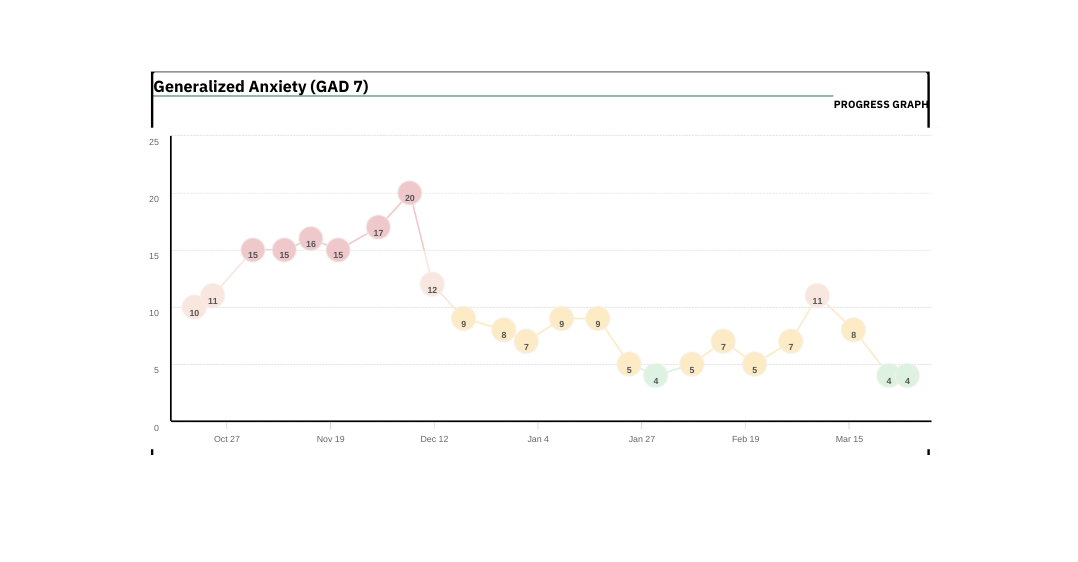
- GAD-7 to track anxiety
- PHQ-9 to track mood and depression
- WSAS to track how well you are doing at work and in daily life
We also use a few more tools specific to your situation, like the ASRS, BADS, and QFV-14. These help us understand your unique challenges and guide treatment. Do you have any questions?”
After answering Malcom’s questions, the therapist sent him the questionnaires to fill out either during the session or soon after. These initial scores became the starting point for measuring his progress, also referred to as the baseline.
Tracking Symptoms and Changes
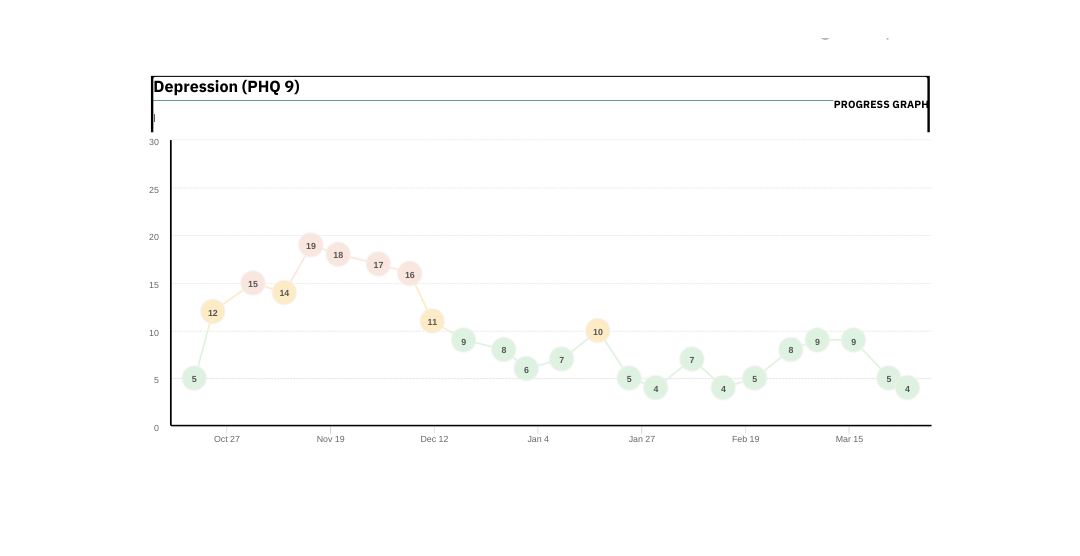
As therapy continues, the therapist keeps collecting and briefly discussing the results to watch for changes.
It is important to remember:
- Numbers do not tell the whole story. Not everything that is important can be measured, and not everything we can measure is important.
- Life events can impact symptoms. For example, losing a loved one might worsen depression, but that does not mean therapy is not helping.
In Malcom’s case, a serious health issue caused his anxiety to spike. The therapist adjusted the treatment to help Malcom manage his anxious thoughts and feelings.
Another challenge in treating depression is that people often see things through a negative lens. This negative thinking can affect how they view their symptom scores or setbacks. Here, techniques like guided discovery or weighing the pros and cons can help the client look at things more objectively.
Handling Sudden Setbacks
 Regular tracking also helps the therapist spot sudden changes. If a client’s scores show a big jump or drop, it is a sign to check in.
Regular tracking also helps the therapist spot sudden changes. If a client’s scores show a big jump or drop, it is a sign to check in.
For Malcom, a new health diagnosis led to a noticeable increase in anxiety and difficulty functioning. When the therapist asked more questions, they discovered that Malcom was rating his functioning based on how he felt, not what he was actually able to do.
For example, Malcom had not cleaned his room for three days—not because he could not, but because he had been working extremely long shifts. Feeling exhausted, he mistakenly believed he was “failing” in daily tasks.
This conversation helped Malcom see the difference between being temporarily overwhelmed and truly unable to complete basic household tasks. Future questionnaire results became more accurate because he better understood what the questions were really asking.
Wrapping Up Treatment: A Visual Summary
At the end of therapy, the therapist created a report showing Malcom’s progress over time—a visual timeline of improvement.
This report served two purposes:
- It gave Malcom clear evidence of how much he had grown and improved.
- It became part of his relapse prevention plan, reminding him of what he had achieved and what strategies helped him get there.
In Malcom’s case, seeing his journey mapped out visually reinforced his sense of accomplishment and highlighted areas that still needed attention.
Measurement-based care plays a powerful role in treating depression. By combining regular tracking with personalized conversations, therapists can tailor treatment, catch setbacks early, and help clients see their progress in a meaningful way.
Malcom’s story shows how using these tools—not just as numbers, but as starting points for deeper conversations—can support healing, growth, and resilience.



